Surgical thyroidectomy is a highly effective treatment for hyperthyroidism in cats. While thyroidectomy is most often successful, it can be associated with significant morbidity and mortality (1-6).
Many potential complications are associated with thyroidectomy, including hypoparathyroidism, Horner's syndrome, laryngeal paralysis, and persistent or recurrent hyperthyroidism. The most serious complication is hypocalcemia, which develops after the parathyroid glands are injured, devascularized, or inadvertently removed in the course of bilateral thyroidectomy. Since only one parathyroid gland is required for maintenance of normocalcemia, hypoparathyroidism develops only in cats treated with bilateral thyroidectomy (4-6).
Pathogenesis of hypoparathyroidism (calcium crisis) after thyroidectomy
Hypocalcemia is the most serious complication associated with thyroidectomy. This adverse effect develops almost exclusively in hyperthyroid cats with bilateral thyroid disease who must have both thyroid lobes removed (bilateral or total thyroidectomy).
Under normal circumstances, the circulating calcium concentration is tightly regulated to remain within a narrow normal range, as calcium is required both for adequate muscle and nerve function. When circulating calcium falls, the parathyroid glands secrete parathyroid hormone (PTH), which leads to an increase in serum calcium concentration back to normal (7). PTH acts on several organs to increase calcium levels, including the intestinal tract, kidney, and bone.
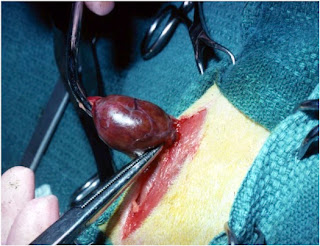
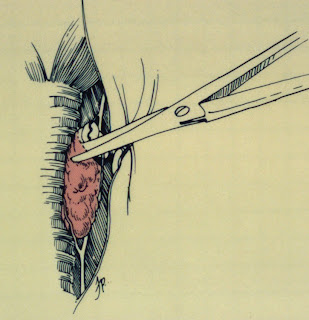
A discussed in my recent blog post on thyroid and parathyroid anatomy, the 4 parathyroid glands are located within or around the cat’s thyroid gland (the prefix para is from Greek, meaning “at or to one side of, beside, side by side”). However, only the external parathyroid glands will be visible at time of thyroidectomy, whereas the internal parathyroid gland will be embedded within the tumor itself (Figure 1).
Clinical signs of hypoparathyroidism (calcium crisis) in cats
Hypocalcemia causes the major clinical manifestations of hypoparathyroidism by increasing the excitability of both the central and peripheral nervous systems (7-10).
Early signs of hypocalcemia due to iatrogenic hypoparathyroidism include anxiety, appetite loss, depression and weakness, twitching, muscle tremors, and facial itch (4-10). Later in the course of hypoparathyroidism, these signs can progress to tetany, collapse, and seizures—hence, the importance of monitoring serum calcium levels during the postoperative period.
Monitoring for hypoparathyroidism after thyroidectomy
After bilateral thyroidectomy, the serum calcium concentration should be monitored on a daily basis until it has stabilized within the normal range. In most cats with iatrogenic hypoparathyroidism, clinical signs associated with hypocalcemia will develop within 1 to 3 days of surgery, but it may take as long as 5 days in some cats (4-10).
Although mild hypocalcemia (6.5-7.5 mg/dl) is a common finding during this immediate postoperative period, laboratory evidence of hypocalcemia alone does not require treatment. However, if accompanying signs of muscle tremors, tetany, or convulsions develop, therapy with vitamin D and calcium is indicated (7-12).
Treating hypoparathyroidism
If symptomatic hypocalcemia develops, the cat needs to be treated with large doses of calcium and vitamin D. Calcium is initially administered as an intravenous infusion, followed by daily oral administration. Large doses of oral vitamin D also need to be given daily to increase the intestinal absorption of calcium (7-12). Supplementation with calcium and vitamin D may be needed for only a few days or for the rest of the cat’s life, depending on the extent of damage to the parathyroid glands.
Although hypoparathyroidism may be permanent in some cats, spontaneous recovery of parathyroid function usually occurs days to months after surgery. Therefore, in most cats with surgically-induced hypoparathyroidism, oral calcium and vitamin D supplementation can eventually be tapered and withdrawn (typically, after a few weeks of treatment).
In most cases, such transient hypoparathyroidism probably results from reversible parathyroid damage and ischemia incurred during surgery. Alternatively, accessory parathyroid tissue may secrete PTH and compensate for the damaged parathyroid glands to maintain normocalcemia, or accommodation of calcium-regulating mechanisms in the absence of PTH may occur (7,13).
Incidence of postoperative hypoparathyroidism
Several studies have evaluated the incidence of hypoparathyroidism after thyroidectomy in cats. In an early study (14), 4 out of 53 cats (7.5%) that had a total thyroidectomy performed with an intracapsular technique developed hypoparathyroidism.
A much higher rate was found in another study that compared the complication between different surgical techniques (15). In that study, extracapsular dissection resulted in an 82% incidence of hypocalcemia, whereas intracapsular dissection resulted in a 36% incidence of hypocalcemia. Staged bilateral thyroidectomy, in which two thyroidectomy procedures were performed a few weeks apart, resulted in an 11% incidence of hypocalcemia (15). However, another study found lower (and similar) rates of hypocalcemia between techniques—23% with a modified extracapsular technique and 33% with a modified intracapsular technique (16).
In the most recent study of thyroidectomy in cats, performed using the modified intracapsular dissection technique, a very low incidence of hypoparathyroidism was reported (17). In that study, only 5 (5.8%) of 86 cats developed postoperative hypocalcemia and none required permanent treatment with calcium and vitamin D.
Bottom Line
No matter which surgical technique is chosen, hypoparathyroidism will develop in a significant proportion of cats treated with bilateral thyroidectomy. However, the very low occurrence of postoperative hypocalcemia in some, but not all, studies suggests that surgeon experience may be the most important factor in determining the outcome for hyperthyroid cats undergoing thyroidectomy.
References:
- Mooney CT, Peterson ME. Feline hyperthyroidism In: Mooney CT,Peterson ME, eds. BSAVA Manual of Canine and Feline Endocrinology. Fourth ed. Quedgeley, Gloucester: British Small Animal Veterinary Association. 2012;92-110.
- Baral RM, Peterson ME. Thyroid gland disorders In: Little SE, ed. The Cat: Clinical Medicine and Management. St. Louis: Elsevier Saunders, 2012;571-592.
- Panciera DL, Peterson ME, Birchard, SJ: Diseases of the thyroid gland. In: Birchard SJ, Sherding RG (eds): Manual of Small Animal Practice (Third Edition), Philadelphia, Saunders Elsevier, pp 327-342, 2006.
- Flanders JA. Surgical therapy of the thyroid. Veterinary Clinics of North America. Small Animal Practice 1994;24:607–621.
- Padgett S. Feline thyroid surgery. Veterinary Clinics of North America. Small Animal Practice 2002;32:851–859.
- Birchard, SJ. Thyroidectomy in the cat. Clinical Techniques in Small Animal Practice 2006;21:29-33.
- Baral RM. Disorders of calcium metabolism In: Little SE, ed. The Cat: Clinical Medicine and Management. St. Louis: Elsevier Saunders, 2012;625-642.
- Peterson ME. Hypoparathyroidism, in Kirk RW (ed): Current Veterinary Therapy IX. Philadelphia, WB Saunders. 1986; 1039-1045.
- Peterson ME. Hypoparathyroidism and other causes of hypocalcemia in cats, in Kirk RW (ed): Current Veterinary Therapy XI. Philadelphia, WB Saunders. 1992; 376-379.
- Skelly BJ. Hypoparathyroidism In: Mooney CT, Peterson ME, eds. BSAVA Manual of Canine and Feline Endocrinology. Quedgeley, Gloucester: British Small Animal Veterinary Association. 2012;56-62.
- Chew D, Nagode L. Treatment of hypoparathyroidism, in Bonagura JD (ed): Kirk’s Current Veterinary Therapy XIII. Philadelphia, WB Saunders. 2000; 340-345.
- Henderson AK, Mahony O. Hypoparathyroidism: treatment. Compend Contin Educ Vet 2005; April:280-287.
- Flanders JA, Neth S, Erb HN, et al. Functional analysis of ectopic parathyroid activity in cats. Am J Vet Res. 1991 Aug;52(8):1336-40.
- Birchard SJ, Peterson ME, Jacobson A. Surgical treatment of feline hyperthyroidism: Results of 85 cases. Journal of the American Animal Hospital Association 1984;20:705-709.
- Flanders JA, Harvey HJ, Erb HN. Feline thyroidectomy. A comparison of postoperative hypocalcemia associated with three different surgical techniques. Veterinary Surgery 1987;16:362–366.
- Welches CD, Scavelli TD, Matthiesen DT, Peterson ME. Occurrence of problems after three techniques of bilateral thyroidectomy in cats. Veterinary Surgery 1989;18:392-396.
- Naan EC, Kirpensteijn J, Kooistra HS, et al. Results of thyroidectomy in 101 cats with hyperthyroidism. Vet Surg 2006;35:287-293.